A phantom limb is a common phenomenon in patients who have had a limb amputated; it consists of a sensation that the limb is still attached to the body and is the origin of the sensation, even though the limb no longer exists. The missing limb often feels shorter than previously. Often the sensations are painful but can include abnormal temperature sensations, itch or tingling. Phantom pains are often described as having a burning, aching or nasty sensation that can be severe or excruciatingly painful. They are often difficult to treat, but the frequency of attacks tends to decrease with the passage of time. Phantom pain, like causalgia, can be made worse by stress and anxiety. The Neuroma Hypothesis One possible reason for phantom pain is the development of a neuroma at the site where limb nerves have been transected and unable to regrow except into the local stump. The nerve endings in the neuroma are sensitive and sometimes express adrenoceptors, which may be the reason why stress and anxiety make the pain worse. So when adrenaline is circulating the nerve endings become more active and the brain 'sees' the sensory input as pain arising from the amputated limb. It is known however that surgical attempts to remove the neuroma usually make the phantom pains worse, and modern studies have suggested alternative mechanisms that place the origin of phantom sensations within the brain rather than in the neuroma. Patients with spinal cord injuries also experience phantom pains, which can be more disabling than the paralysis that affects these patients. The pains may be intractable and chronic, and often not responsive to the common anaglesics. |
Cortical Reorganisation The more modern view of phantom pain arises from an understanding of how our experience of bodily sensations depend upon a wide network of connections between neurones, including the primary somatosensory area of the cerebral cortex. It is known for example that there is a considerable reorganisation of the primary cortical receiving area that previously dealt with neural inputs from the amputated limb. It has been suggested that phantom sensations arise because of the substantial reorganisation of the primary somatosensory cortex following amputation, and some experimenters have shown that light tactile stimulation of the face can give rise to the perception that the phantom limb is being touched. However the main sensory experience present in patients with demonstrable corticl reorganisation was phantom pain. The reorganisation of the cerebral cortex following amputation of a limb is thought to be associated with changes in other neural circuits outside the cortex iteself. So the modern view is that phantom pain arises because of a reorgansiation of neural networks with several areas of the brain as a consequence of the loss of afferent input from the detached limb. It remains unclear as to why pain is the almost inevitable result of the reorganisation of central pathways. For a further consideration of the ability of the central nervous system to reorganise its pathways, go to the section on Neuroplasticity. However it is also clear that there are major neuroplastic changes at the level of the primary afferents following nerve injury: |
Biochemical, anatomical and physiological changes of lesioned primary afferent neurons following nerve lesion and the subsequent central changes. 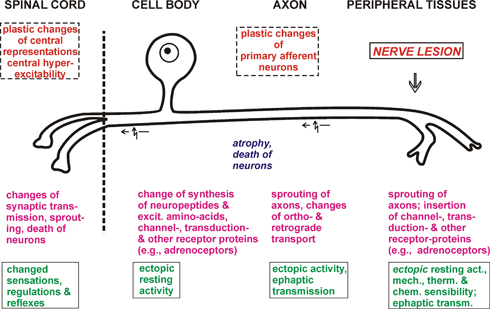
(http://www.physiologie.uni-kiel.de/homepages_mitarbeiter/jaenig/neu/hompage.html) This diagram show some of the changes that appear to be relevant to the neuropathic pain that occurs after nerve injury. |
|